Groundbreaking Study Reveals How Cancer Cells Disrupt Blood Systems
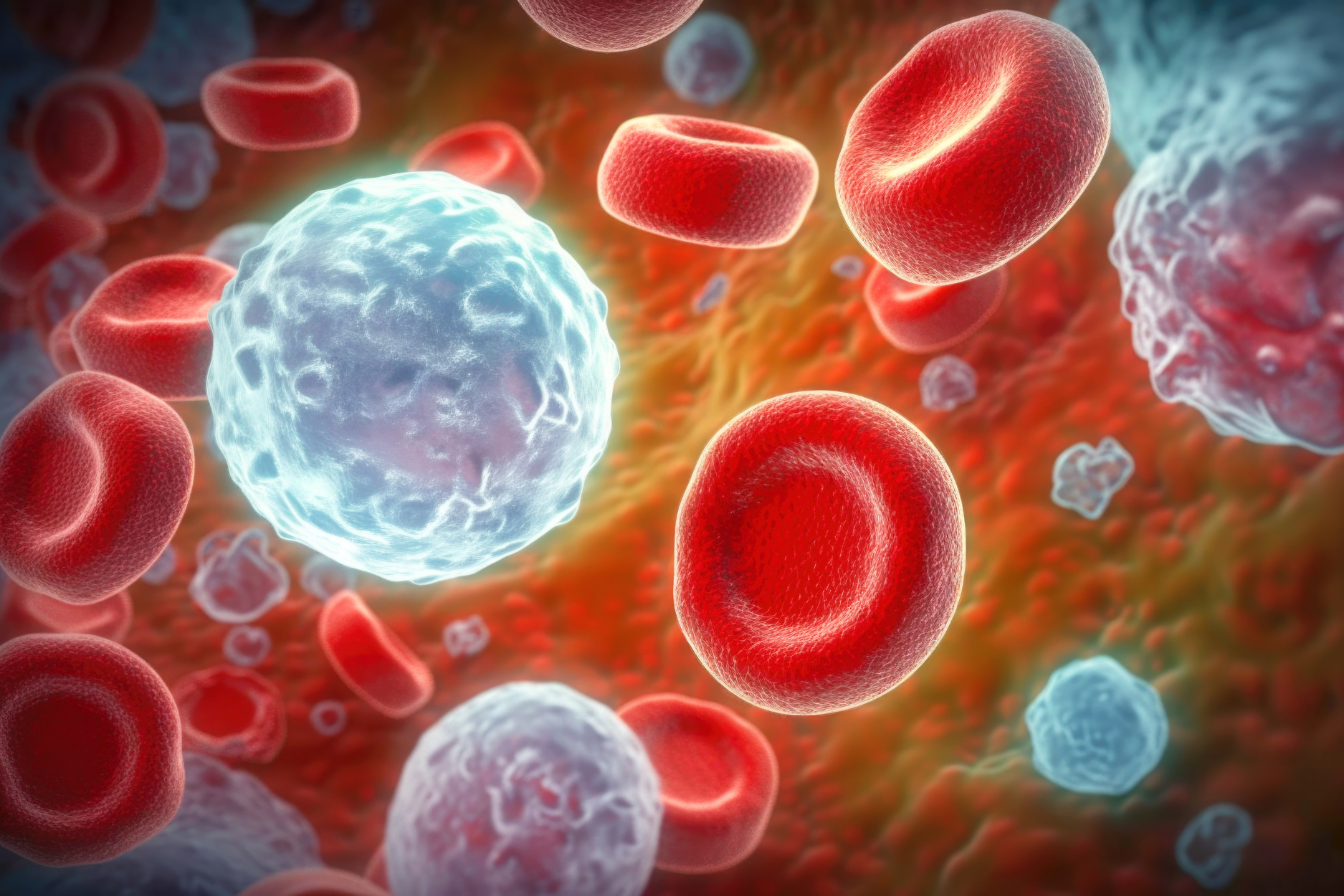
A groundbreaking study led by researchers at Brown University has unveiled how mutated blood cancer cells can have profound and widespread effects on the entire blood-forming system, not just on nearby cells. This research, published in the journal Blood by the American Society of Hematology, sheds new light on the systemic impact of cancerous cells in the body.
Under the leadership of Associate Professor Patrycja Dubielecka from Brown's Warren Alpert Medical School, the research team discovered that even a small number of these mutated cells can significantly disturb the blood-producing process and bone health. Dubielecka, who also co-leads the Cancer Biology Program at Brown’s Legorreta Cancer Center, expressed surprise at the extent of these changes.
“The changes observed were far more significant than anticipated,” Dubielecka stated. This insight has crucial implications for treating blood cancers. She emphasizes the importance of understanding the molecular changes in non-mutated cells that are affected by the presence of cancer cells, which could pave the way for new therapeutic approaches.
The study's lead author, Dennis Bonal, a postdoctoral fellow at Brown, developed a mouse model that allows for precise tracking of introduced cancer cells. This model simulates the human condition where cancer evolves over time, providing a valuable tool for researchers.
Through this model, the researchers introduced varied amounts of cancer cells into mice, observing them over eight months. They noted that a particular gene mutation, JAK2, caused significant molecular mimicry between mutated and non-mutated cells. This discovery suggests a need to rethink current treatment strategies, which often involve 'watchful waiting' rather than aggressive intervention.
Dubielecka argues for a shift in strategy: “Early detection of mutated blood cancer cells should prompt efforts to reduce the mutated clone's presence to prevent irreversible damage.”
As the team continues their research, they aim to explore the changes in non-mutated cells further, with hopes of reversing the damage caused by mutated cells. This study was supported by funding from the National Cancer Institute and the National Institute of General Medicine.