When The Immune System Turns on You: New Clues to Allergies, Asthma, and Autoimmunity

Your immune system is built to protect you. But what happens when it becomes the attacker?
In a revealing new study from Harvard Medical School, researchers are zooming in on how rogue B cells, crucial immune defenders, may play a central role in chronic diseases like allergies, asthma, and autoimmune disorders. The findings could transform how we treat these conditions, shifting the focus from symptom relief to immune system reprogramming.
Led by immunologist Dr. Duane Wesemann, the research team is unpicking the molecular mechanics behind how B cells learn to distinguish friend from foe, and what happens when that process goes wrong.
“We’re trying to understand the immune system at its decision-making core,” Wesemann explains. “Most of the time, it protects us. But sometimes, it targets things it shouldn’t, like pollen, food proteins, or even the body’s own tissues.”
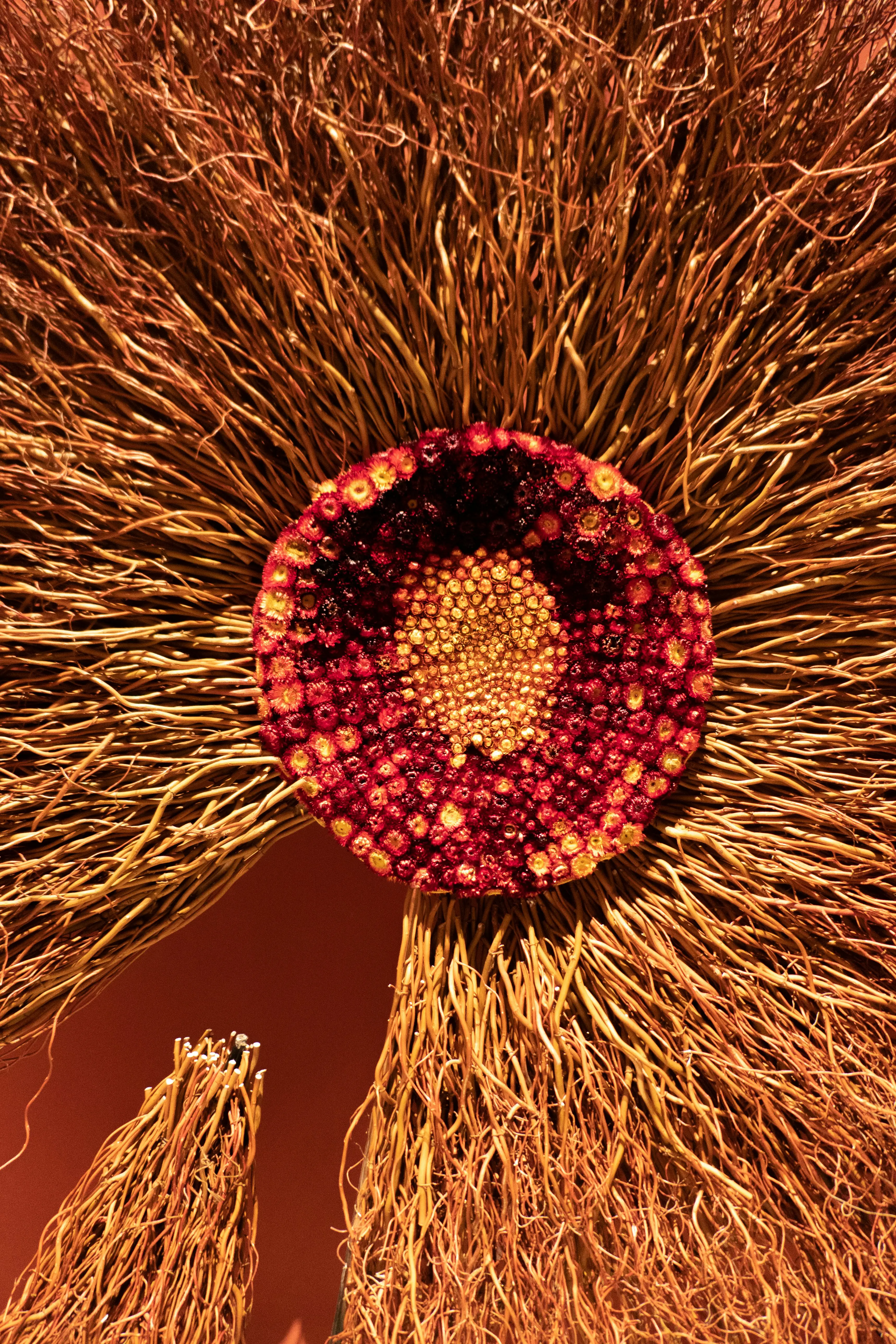
At the center of their investigation is the germinal center, a specialized structure in lymph nodes where B cells evolve and mature. Here, B cells are trained to recognize invaders like viruses and bacteria. But during this training process, mutations occur. If these rogue versions escape the body’s internal checks and balances, they can turn on harmless substances, or worse, the body itself.
This cellular betrayal is the root of conditions like lupus, rheumatoid arthritis, food allergies, and asthma. What makes Wesemann’s work stand out is the focus on catching the problem at its source, rather than downstream.
By identifying the early signals that flag a B cell as “going rogue,” his lab hopes to intercept these cells before they cause harm, possibly using future therapies to retrain or remove them.
Their research is already yielding critical insights. The team has mapped how environmental factors like infections, diet, and even stress can influence the germinal center environment, altering immune decisions in lasting ways. This could help explain why allergies and autoimmune disorders have skyrocketed in recent decades, and why some people are more vulnerable than others.
“If we can understand why certain B cells slip through the cracks, we can design smarter treatments, or even prevent these disorders entirely,” says Wesemann.
The implications are massive. One in ten people worldwide now suffers from autoimmune disease. Allergies are exploding in both industrialized and developing nations. For many, the immune system is no longer just a shield, it’s a ticking time bomb.
But with deeper insight comes new hope.
Wesemann’s lab is part of a growing movement in immunology that views the immune system not just as a battleground, but as an adaptable, reprogrammable system. And if we can learn to recalibrate it, to remind it what truly matters, the next generation of treatments could be far more precise, and far less punishing.